👋 Welcome to Starting Early. Every other week, we spotlight new reports, useful news, engaging interviews with people doing important work in the field, and interesting takes on issues that matter.
Last spring, Burke staff read about a class taught by Professor Heather Howard at Princeton that empowers undergraduates to explore inequities in New Jersey’s healthcare system and propose policy solutions. Turquoise Brewington, a brilliant junior in the class, was evaluating how to improve outcomes for Black mothers by expanding Medicaid coverage for home births and midwives. Now we welcome Turquoise as our maternal infant health intern.
We’re also pleased to report that a crucial policy recommendation was realized last week when New Jersey became only the second state to expand Medicaid coverage for 365 days postpartum. This will bring continuity in coverage for 9,000 women who would have been cut off after 60 days and is a national model for improving maternal and infant health.
Read on and click the links to go deeper.
1. Advancing midwifery care in the United States
Turquoise and the Burke team embarked on a research project to better understand the practice of midwifery in New Jersey and promote opportunities to expand and diversify the midwife workforce.
The problem: High spending on maternity care doesn’t always mean better maternal health outcomes in the US — especially for women of color.
We’re studying the midwifery workforce and looking for actionable recommendations to raise the visibility of this longstanding health profession and develop its untapped potential to reduce racial disparities in maternal care and improve maternal health outcomes.
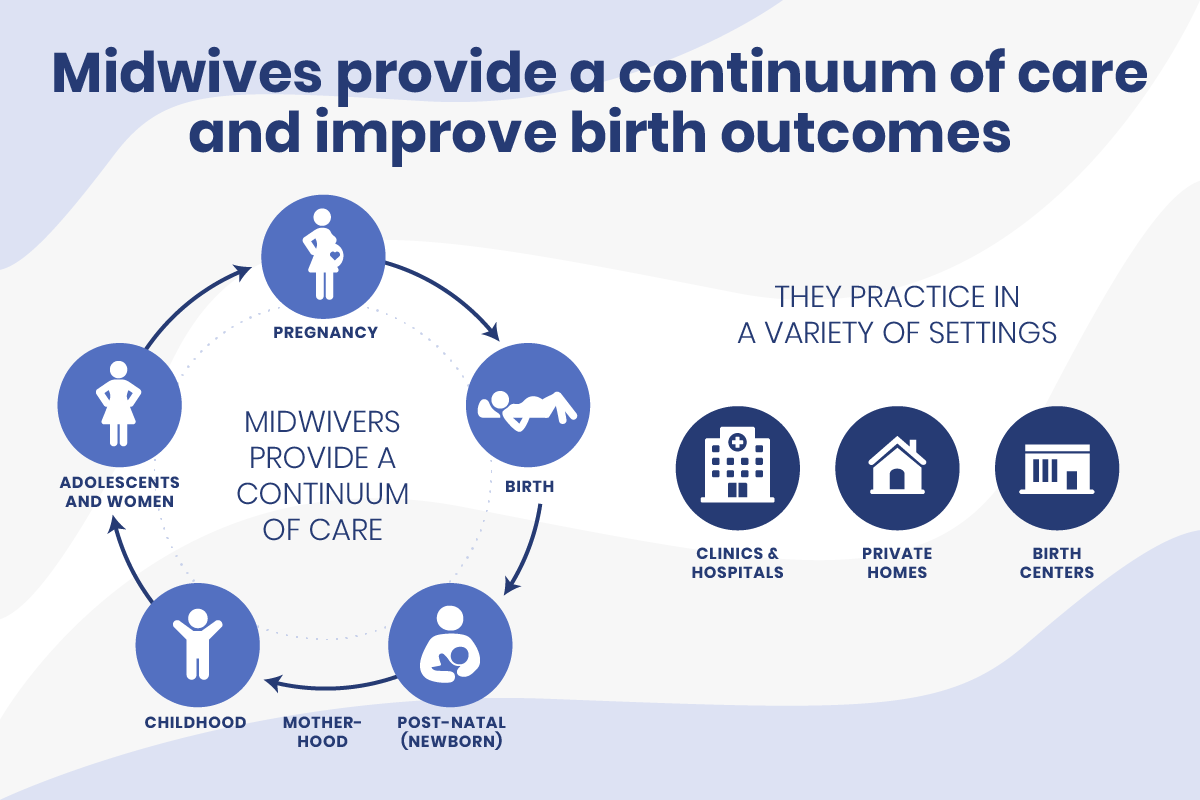
Why midwives matter: Midwives are traditional care providers for mothers and children, going back centuries. Midwives assist in childbirth as well as during pregnancy and the postpartum period. They specialize in individual care and can deliver babies in varied settings. Unlike doulas or community health workers, midwives are clinical providers.
- Midwife-led maternity care results in substantially higher rates of vaginal delivery and lower rates of C-sections, as well as significantly lower rates of preterm births and low-birthweight infants compared to other maternity models.
- A recent report from the Commonwealth Fund notes that midwives also have the capacity to contribute to health equity by providing culturally-congruent care.
Challenges remain: By 2019, births among people of color had risen to almost half of US births, but the nurse midwifery workforce remains almost 90% white.
“Midwifery has been an ‘invisible profession’ for too long,” shared Linda Locke, a nurse midwife and former chief of midwifery at St. Joseph’s Regional Medical Center in Paterson. “Many people in the United States, including people in communities of color, don’t know what midwives are or what we do. In addition to getting out more information about midwifery to everyone, there is a need to reach out to students, and especially students in communities of color, as early as high school, to let them know that midwifery is a viable career.”
What we’ve learned: In addition to researching midwifery practice, education, and outcomes, we spoke with 15 practitioners, midwifery students, and maternal health stakeholders working in New Jersey and across the country.
We learned about:
- Reducing educational and financial obstacles to studying midwifery
- Diversifying the midwifery workforce by expanding mentorship and creating career pathways for doulas and community health workers to become midwives
- Increasing opportunities for midwife clinical training, including in team-based and community-embedded settings
- Changing systems to increase insurance reimbursement rates for midwifery services and develop sustainable reimbursement models for midwifery care
We’re excited to be planning a convening for stakeholders in early 2022 before publishing a final report.
The bottom line: Midwives can make the experience of giving birth safer and more cost-effective. The COVID-19 pandemic magnifies the demand for midwives throughout the US, as pregnant women increasingly look to community-based settings like birthing centers for care that meets their needs. Growing the perinatal workforce through intentional investment in programs designed to diversify the midwifery workforce could be especially valuable.
2. Transforming pediatric care for families

The pediatric setting plus 13 well-child visits during the first 3 years of a child’s life have the potential to introduce families to useful knowledge and critical resources. Reaching children and families in this important time gives them the best chance of success in development and life.
But, but, but: Busy pediatricians usually only have 15 minutes at a time to connect with families.
Expanding the care team: The evidence-based HealthySteps pediatric care model integrates a child-development specialist into the primary pediatric team.
- HealthySteps Specialists act as a single, family-facing focal point. They build trust among families with tailored referrals to community resources, screening for family needs, and a support line to address non-medical questions around parenting and development.
- The program helps increase childhood immunization and development-screening rates, lengthen breastfeeding duration, improve identification and early intervention with maternal mental health and substance-use disorders, reduce ER visits, and even help participants get a better night’s sleep.
Medicaid funding allows HealthySteps to expand the care team and work with parents and young children beyond what Medicaid traditionally involves, including behavioral health and helping connect parents to housing, transportation, and good nutrition — all of which improve lifelong health.
Piloting HealthySteps in New Jersey: Despite battling the pandemic, Dr. Judy Aschner, chair of pediatrics and physician-in-chief at Hackensack Meridian Health, was committed to implementing HealthySteps there. Hackensack hired a full team of 3 child development specialists embedded in 4 pediatric practices that now serve about 2,500 patients up to age 3.
- From its start in February 2021, the program served nearly 1,250 families. HealthySteps Specialists made over 500 referrals to community resources (food insecurity was the top reason) and every child received at least one developmental and social emotional screening.
- Having HS Specialists serve 2,000 families, resulting in $245,380 annual savings to NJ Medicaid.
The bottom line: Parents face social and logistical barriers not always seen as directly related to a child’s health or development, but still problematic.
“Food insecurity and financial hardships are major challenges for families who are undocumented and have limited resources and access to support,” shared Ediza Lahoz Valentino, a Healthy Steps Specialist. “Transportation, for example, is a big problem. As part of HealthySteps, we get people to their well-child visits.”
Watch Dr. Rahil Briggs, national director, HealthySteps at ZERO TO THREE, and Dr. Judy Aschner, of Hackensack Meridian Health, discuss the importance of the HealthySteps program with NJTV’s Steve Adubato.
3. What inspires us
Lifelines: A Doctor’s Journey in the Fight for Public Health by Dr. Leana Wen
Burke’s team of public health aficionados is raving about Dr. Leana Wen’s memoir. It’s a powerful immigrant story — from Shanghai to a small town in Utah to Los Angeles — and love letter to public health that gets inside of the woman leading Baltimore’s health department. She shares her life journey and leadership, tested by Freddie Gray’s death and taking on the opioid crisis.
Dr. Wen takes us with her, not just on her remarkable life journey helped along by Medicaid, WIC, and public housing, but also into an exploration of broken systems and inequities deeply entrenched in our health system.
In a conversation with the Washington Post, Dr. Wen shared:
“One of the stories I recount early in ‘Lifelines’ is about how I watched a neighbor’s child, who was just a couple of years younger than me, die in front of me because his grandmother was too afraid to call for help for his health because she was afraid that the immigration authorities would come, and that would result in the entire family being deported. You can imagine from an early age, watching a child die, in this case, from asthma right in front of me, had such a profound impact on what I understood about our health care system, that health care in this country is not valued to be the right that it needs to be, and that our society treats people very differently, depending on who they are and where they come from.”
Actionable public health initiatives:
- B’more for Healthy Babies: The innovative initiative led by the Baltimore City Health Department and the Family League of Baltimore reduced infant mortality by 38% in 7 years.
- Naloxone distribution: Over 3 years, the program saved over 3,000 lives from the opioid epidemic.
Subscribe to Dr. Wen’s Washington Post column.
