👋 Welcome to Starting Early. Every other week, we spotlight new reports, useful news, engaging interviews with people doing important work, and interesting takes on maternal health and early childhood development issues.
This week’s issue is the second of a two-part series discussing Medicaid. In our first issue of the series, we gave an overview of Medicaid and its contributions to the health and wellbeing of 78 million people in the US, which continues to experience very high health costs and, for too many people, disappointing results. Today, we delve into Medicaid innovations.
Jointly funded by the federal government and states, Medicaid must provide certain coverage to specific categories of people under federal law. Beyond that, each state determines Medicaid eligibility and services. This results in significant state-to-state differences. That’s good and bad: It creates disparities across the US, but also gives states flexibility to implement innovative solutions to serve community needs.
New Jersey uses Medicaid as a powerful tool to improve maternal and child health and address the state’s high maternal mortality rate, especially among Black women. In the state budget Gov. Phil Murphy recently proposed for the next fiscal year, Medicaid spending would rise by $15 million to increase the reimbursement rate for midwives, doulas, and clinicians. This is a necessary reform from the standpoint of improving healthcare access, quality, and outcomes — and more is needed.
1 big thing: Federal waivers advance health equity in Medicaid
States have wide latitude in designing their Medicaid programs and can use such tools as federal Section 1115 waivers to tailor services to meet various needs. Medicaid Section 1115 Demonstration Waivers allow states to disregard certain federal requirements so they can test pilot programs that could better serve people enrolled in Medicaid or expand eligibility and coverage.
While the previous administration’s Section 1115 waiver policy restricted eligibility and limited Medicaid spending, the Biden Administration takes an approach aimed at expanding coverage to make quality healthcare available to more people.
States are using Section 1115 waivers to:
- Expand opioid-use and substance-use disorder treatment services
- Help individuals with HIV/AIDS and behavioral health issues, newborns, and caretakers
- Reduce copays, premiums, and prescription costs
- Increase incentives for healthy behavior, like completing health screenings
Why it matters: People whose low incomes make them eligible for Medicaid often are those who suffer the worst outcomes, stemming from current and former social, economic, and health policies disadvantaging people of color and other marginalized groups. Section 1115 waivers can lead to state-level reforms that advance health equity and address health disparities and could become federal requirements for every state. As they develop strategies to improve healthcare delivery, benefits, and coverage, many states are addressing social determinants of health — such as access to nutrition, transportation, and stable housing — collaborating with community stakeholders, and using data to evaluate health equity priorities.
- Reminder: 80% of health outcomes are determined by social and economic factors, and not strictly “medical” issues.
Go deeper: Read Princeton Professor Heather Howard’s (@HeatherHHoward) informative Twitter thread on Section 1115 waivers and why Medicaid’s size and scope makes it a vital lever for improving services.
2. Transforming behavioral health in California

During traditional pediatric visits, providers often lack the time to address important issues relevant to healthy child development that may require additional time beyond a traditional well-child visit. HealthySteps, a program of ZERO TO THREE, fills this gap by integrating a behavioral health specialist within a pediatric primary care team. We sat down with Jennifer Tracey, Senior Director of Growth and Sustainability for HealthySteps to discuss the model and national efforts to secure sustainable funding for program sites.
A team-based approach: “The HealthySteps Specialists are an extension of the primary care team; they give additional support to families with young children. Specialists can provide short-term behavioral and developmental consultations and link families to services within the community. The Specialists are another member of the primary care team that can serve as an advocate for families and answer developmental questions beyond what the pediatrician has the time to do in an already busy well-child visit.”
We asked Jennifer about innovative billing approaches and she shared this example: “In 2019, we created a dyadic billing proposal with some of our California partners called Babies Don’t Go to the Doctor by Themselves. As a result of the proposal and subsequent health plan conversations, San Francisco Health Plan developed an innovative way to pay for preventive behavioral health well-child visits (inclusive of certain HealthySteps visits), which are not traditionally covered by state Medicaid agencies or health plans.”
A game-changing development: San Francisco Health Plan’s adoption of the dyadic billing proposal helped inform California’s new Medicaid benefit for dyadic care, which serves children’s and caregivers’ behavioral health needs simultaneously. California has dedicated $800 million over four years to the new benefit.
- Starting January 2023, caregivers attending a well visit with a child up to age 21 will receive integrated screenings and services for physical and behavioral health concerns and assistance connecting to such wraparound services as food vouchers and housing assistance.
- This new Medicaid benefit — the first of its kind in the US— will reimburse healthcare providers for such evidence-based, dyadic care approaches as HealthySteps.
Across the US, states are increasingly using similar innovative strategies to improve the health and wellbeing of those covered by their Medicaid programs. We’ll be watching California’s bold investment in dyadic care as a model for other states.
One smile to go: Sharing healthcare stories
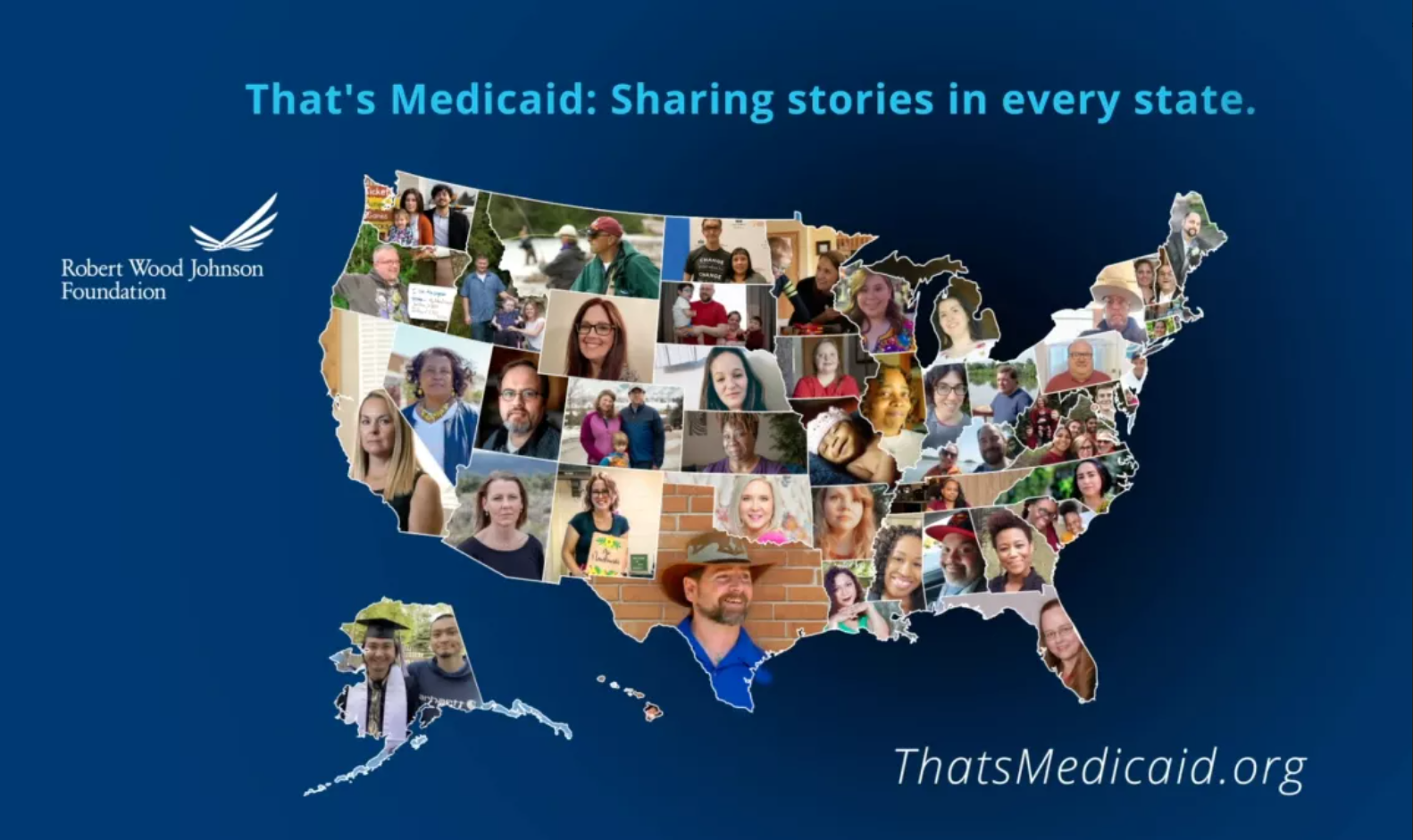
As part of its work to build a Culture of Health in the US and eliminate disparities, The Robert Wood Johnson Foundation funds research on Medicaid, advocates for closing the Medicaid Coverage Gap, and supports Medicaid-specific programs.
To show the importance of Medicaid, RWJF centers the voices of participants through a storytelling project, That’s Medicaid. Some highlights:
- Supporting children’s futures in Missouri: When Sonia gained custody of her great grandnephew, she enrolled in Medicaid to cover his extensive medical needs. Amir was born with developmental disabilities requiring therapy and other services Sonia couldn’t afford. “Thanks to Medicaid,” she says, “I’m able to witness Amir’s development improve. I expect him to have a very decent quality of life.”
- Bolstering mental health in Wyoming: The pandemic caused Danielle financial challenges that severely eroded her emotional and mental wellbeing. After signing up for Medicaid, Danielle connected with a primary care provider who prescribed anti-depressants and with a therapist who provided counseling. “I’ve been able to be a mom again,” she reflects. “I’ve been able to work again, I’ve been able to feel good about life. I feel like Medicaid has saved my life.”
- Providing high-quality maternal care in Oregon: When Alicia needed health coverage while pregnant with her oldest child, Medicaid assigned a doula to support her through pregnancy, birth, and postpartum care. “Because of this life-changing experience and the amount of help I was offered, I chose to take the path of becoming a doula and working with mothers and families in my community,” Alicia reports.
Follow @ThatsMedicaid on Twitter for more impactful stories.
4. The roundup
Learn about upcoming events, new funding opportunities, and jobs in maternal and infant health and early childhood:
- Supporting childcare providers in New Jersey: The New Jersey Economic Development Authority is hiring a Senior Advisor for Child Care. Apply now to lead the development, rollout, and implementation of new initiatives strengthening the state’s childcare sector.
- Transforming maternal and infant health care: Cape OB/GYN Associates in New Jersey, an Axia Women’s Health Center, seeks a certified nurse midwife for its practice. Apply to join one of the largest women’s health groups in the country and provide quality, compassionate maternal care.
- Helping families thrive: Register for the Center for Child and Family Policy at Duke University’s April 12 virtual convening on best practices for creating a universal system of care to better support young children and their families.
- Developing the doula workforce: Join the Center for Health Care Strategies and the California Health Care Foundation for a March 29 webinar exploring challenges and opportunities to expand the doula workforce. Register to hear best practices from California and New Jersey’s efforts to support doulas.
- Bolstering New Jersey’s public health system: The Robert Wood Johnson Foundation is calling for proposals to create a public health institute in New Jersey. The submission deadline is April 13. For more information, register to attend an applicant webinar on April 1.
